THE RESPIRATORY THERAPY DEPARTMENT
AT MINIDOKA MEMORIAL HOSPITALRespiratory therapists are specially trained healthcare professionals who work with physicians to provide a wide range of respiratory procedures and other services to people with asthma, chronic obstructive pulmonary disease, cystic fibrosis, lung cancer and other lung related conditions. The standards for the Respiratory Therapy department are established by the National Board for Respiratory Care, Inc. and the American Association for Respiratory Care.

THE MMH RESPIRATORY THERAPY DEPARTMENT OFFERS THE FOLLOWING SERVICES:
INPATIENT SERVICES
- Emergency care
- ICU – Critical patient care
- Oxygen administration (via numerous devices, as ordered by a physician).
- Pulmonary hygiene (including chest physiotherapy, cough-assist, suctioning, or use of PEP (Positive Expiratory Pressure) therapy and other patient-use devices for airway clearance)
- Inhaled pulmonary medications (delivered via nebulizer, aerosol, or inhalers)
- Invasive and Non-invasive ventilator support, utilizing the latest technology
- Vapotherm, High flow VNI therapy (High Flow Velocity Nasal Cannula)
OUTPATIENT SERVICES
- Cardiac stress testing
- Pulmonary function testing
- Home Sleep Studies (ACHC Accredited)
- Respiratory Outpatient Clinic (ROC)
- Soon to come: Respiratory COPD Navigator Program (A dedicated trained therapist, assigned to our COPD community, for their journey with this disease)

RESPIRATORY OUTPATIENT CLINIC (ROC)
Minidoka Memorial Hospital offers a Respiratory Outpatient Clinic (ROC) that provides support for newborn to 18 months old with Bronchiolitis, commonly referred to as RSV (Respiratory Syncytial Virus) for the virus that most often causes Bronchiolitis. With a referral from your child’s primary care provider, our team of respiratory therapists will complete an assessment of your child’s condition and then treat accordingly. Treatments include small volume nebulizers and suctioning. These treatments relieve the labored breathing and improve your child’s ability to breathe, sleep, eat and drink. Therefore, helping to avoid additional complications, like dehydration and hospitalization.

BRONCHIOLITIS SYMPTOMS
Bronchiolitis usually begins as a cold and symptoms often include:
- Fever
- Runny nose or nasal stuffiness
- Mild Cough
- Less appetite
- Mild problems breathing
As the virus spreads to the small airways of the lungs (1-3 days later) a whistling sound called wheezing may be heard when the child breathes out. At this time, symptoms worsen and broaden to include:
- Rapid breathing (60-80 breaths per minute)
- Mild to severe breathing problem
- Constant coughing
- Problems eating
- Apnea (babies who were born early or who are under the age of 2 months may stop breathing for short periods of time.)
In healthy infants and children, Bronchiolitis usually goes away on its own, but for many children the symptoms can become severe and hospitalization is required. If your child was diagnosed with Bronchiolitis (RSV) please ask your physician for a referral to our Respiratory Outpatient Clinic for additional treatment.
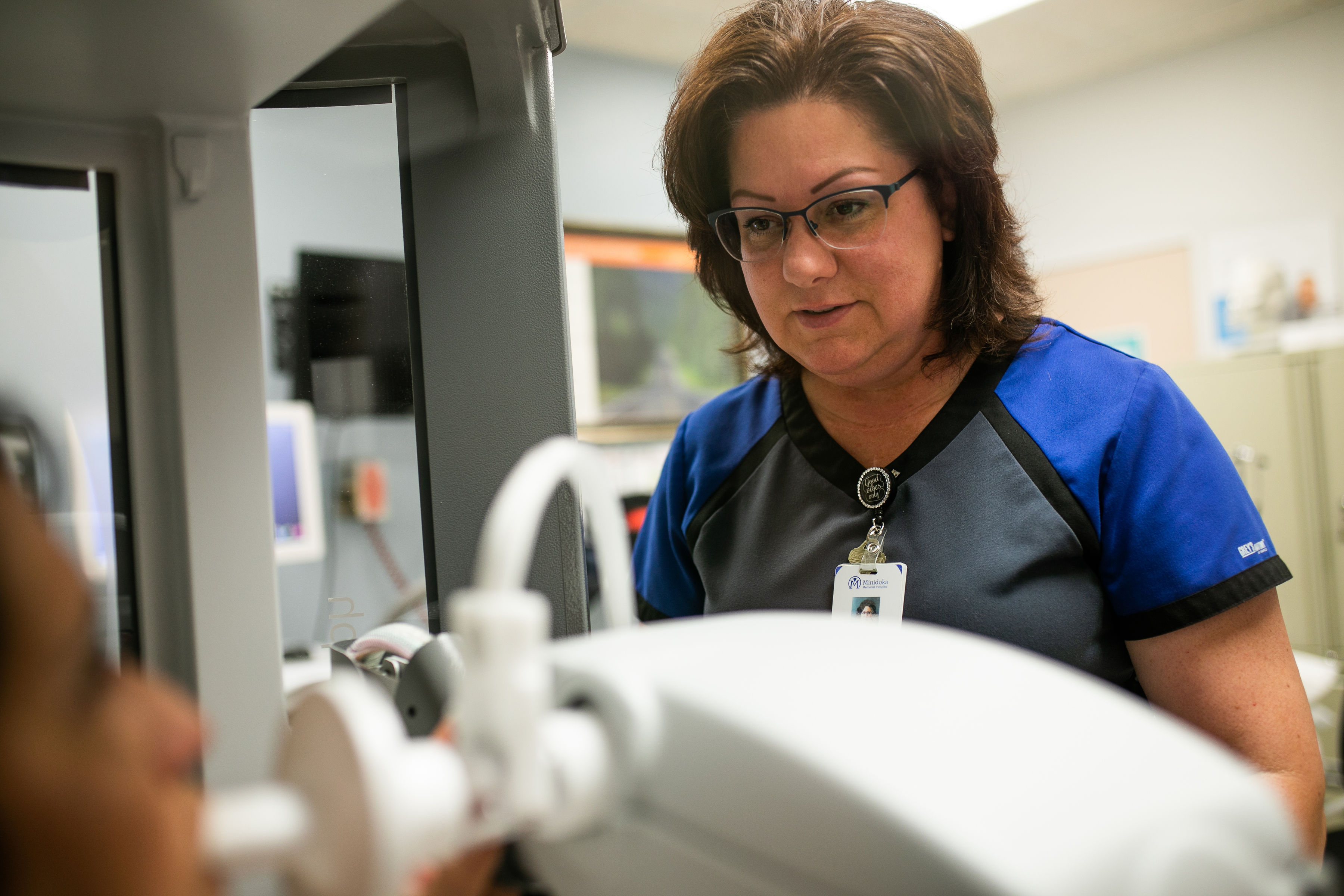
PULMONARY FUNCTION TESTING (PFT)
Pulmonary function tests (PFTs) is a group of tests that measure how well your lungs work. This includes how well you’re able to breathe and how effective your lungs are able to bring oxygen to the rest of your body.
Your doctor may order these tests:
- If you’re having symptoms of lung problems
- If you’re regularly exposed to certain substances in the environment or workplace
- To monitor the course of chronic lung disease, such as asthma or chronic obstructive pulmonary disease (COPD)
- To assess how well your lungs are working before you have surgery
Your doctor will order these tests to determine how your lungs are working. If you already have a condition that’s affecting your lungs, your doctor may order this test to see if the condition is progressing or how it’s responding to treatment.
AT HOME SLEEP TEST
(WHAT YOU NEED TO KNOW)Do you find yourself waking up tired, or maybe with a headache or dry mouth? Obstructive sleep apnea could be to blame. This happens when your breathing is interrupted during sleep, often for more than ten seconds.
At-home sleep apnea testing is an easy, cost-effective way to figure out whether you’re having trouble breathing while sleeping. A home sleep apnea test is a very simplified breathing monitor that tracks your breathing, oxygen levels, and breathing effort while worn. If you are being told that you snore, snort and gasp, if you have disrupted sleep or are sleepy during the day, and you are overweight or obese, an at-home sleep apnea test may be very appropriate for you. Talk with your clinical provider about your options.

THE FACTS
A sleep test is meant to evaluate a patient for sleep apnea, and it monitors breathing parameters, not the sleep itself.
The sleep test won’t analyze how long you’re in light or deep sleep. Instead, it will measure pauses in and absence of breathing, how much effort it takes to breathe and whether your breathing is shallow.
This isn't an over-the-counter test.
Your primary care physician or a physician at a sleep clinic can order it to be taken home.
The sensors include a small probe over your finger that measures oxygen levels.
You’ll insert another mask with tubes into your nostrils and secure it around your ears, similar to an oxygen mask. Another sensor is placed around your chest to measure the rise and fall as you breathe.
Most at-home sleep tests are used just for one night.
It’s also less expensive than a sleep study in a clinic. It’s usually a third to a fifth of the cost of doing an in-lab study, and it’s typically covered by insurance.
With an at-home study, you’ll be in the comfort of your own surroundings.
Which could offer a more accurate reading of how you actually sleep.
After the test, your results will be reviewed by a sleep certified physician and sent to your primary physician.


